
US Vaccine Advisers Just Made a Shocking Decision: Should Your Baby Skip the Hepatitis B Shot? Find Out Now!
NEW YORK (AP) — In a surprising move, a federal vaccine advisory committee has voted to end the longstanding recommendation that all U.S. babies receive the hepatitis B vaccine on their birth day. This decision has ignited a firestorm of criticism from many medical and public health leaders who fear it could have significant implications for public health.
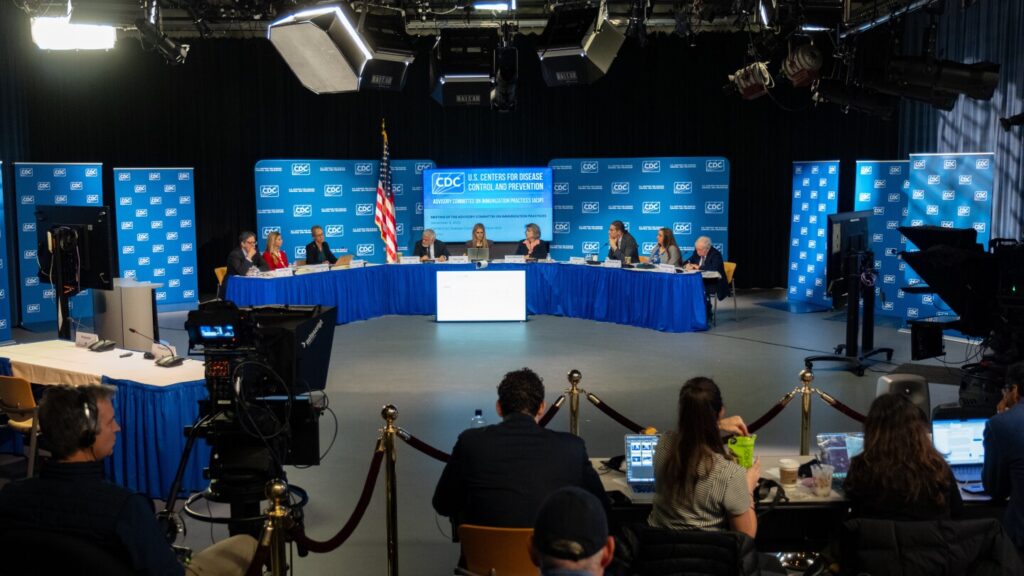
The Advisory Committee on Immunization Practices (ACIP), whose members were all appointed by U.S. Health Secretary Robert F. Kennedy Jr.—a prominent anti-vaccine activist—decided on this change with a vote of 8-3. The new recommendation suggests the birth dose of the hepatitis B vaccine should only be administered to infants whose mothers test positive for the virus or in cases where the mother is untested. Parents will now have to make the decision in consultation with their healthcare providers regarding the birth dose for other newborns, with the committee stating that the vaccination series should begin at two months old if the birth dose is skipped.
Dr. William Schaffner, a vaccine expert from Vanderbilt University who has worked with ACIP for decades, expressed deep concern about the committee's direction, stating, “This is the group that can’t shoot straight.” The hepatitis B vaccine has long been considered a public health triumph, effectively preventing thousands of illnesses and reducing the spread of this serious liver infection.
Historically, the committee's recommendations have been closely followed by healthcare professionals, influencing vaccination programs nationwide. However, the new approach marks a significant departure from a public health strategy that has been in place for over three decades. In 1991, the committee recommended administering the first dose of the hepatitis B vaccine at birth to prevent the infection from setting in, particularly for infants born to infected mothers.
Dr. Cody Meissner, another committee member, cast a dissenting vote, arguing, “We are doing harm by changing this wording.” This sentiment was echoed throughout the meeting, which saw heated discussions about the implications of altering the vaccine's recommended administration timeline. Committee members argued that the risk of infection for most infants is low and expressed concerns that past research supporting the vaccine's safety in newborns was insufficient.
Despite the committee's assertions, many public health experts, including Dr. Peter Hotez of the Texas Children’s Hospital Center for Vaccine Development, have openly criticized ACIP's new direction. Hotez chose not to present his findings before the committee, stating that it has shifted away from evidence-based medicine.
The acting director of the Centers for Disease Control and Prevention (CDC), Jim O’Neill, is expected to make a final decision on whether to accept the committee’s recommendation. This is particularly significant given that the CDC currently has no permanent director, leaving O’Neill with the responsibility of determining future vaccination guidelines.
Pressure from undisclosed stakeholder groups was cited by committee member Vicky Pebsworth as a reason for the rapid reevaluation of the vaccination policy. The absence of a well-defined rationale for the new recommendations, particularly regarding the two-month delay for administering the vaccine, has led to skepticism and concern among health professionals. Dr. Joseph Hibbeln, another committee member, called the proposal “unconscionable” and challenged the lack of supporting data for delaying the vaccine.
Adding to the debate, the committee also passed a proposal suggesting parents consider blood tests to measure whether hepatitis B vaccinations have created protective antibodies. This practice is not standard in pediatric healthcare, and experts warn it could lead to inconsistent assessments of vaccination adequacy.
Republican Sen. Bill Cassidy, a liver specialist and chair of the Senate health committee, criticized the committee's decision, labeling it “a mistake” and warning that it could lead to a resurgence of hepatitis B cases. In a social media statement, Cassidy cautioned that “ending the recommendation for newborns makes it more likely the number of cases will begin to increase again. This makes America sicker.”
The hepatitis B virus can cause serious long-term issues, including liver failure and liver cancer, particularly in infants and children. Historically, timely immunization has been pivotal in preventing the establishment of infection in newborns, contributing to plummeting cases of hepatitis B in children.
The recent shift in policy is not just a medical decision; it reflects broader debates around vaccination practices and public health strategies that could have far-reaching consequences for American families. As the CDC considers the new recommendations, the conversation surrounding vaccination continues to evolve, revealing significant divides in the understanding and acceptance of vaccines among healthcare professionals and the public.




You might also like: